Most of us have heard of the term Adrenal Fatigue. New research indicates that, contrary to the name of the condition, it is not really a case of the adrenal system becoming fatigued, but rather a miscommunication between the brain’s HPA axis (hypothalamus-pituitary-adrenal axis) and the adrenal system because of continuous stress. This leads to a Phase 1, and later Phase 2 Cortisol Imbalance, causing the symptoms we have come to relate to ‘Adrenal Fatigue’.
In this article I provide an overview of the adrenal system, the role cortisol plays in a healthy body, what happens to cause cortisol imbalances in the body, and finally, what can be done to restore the balance back to normal.
What are the adrenal glands and their function?
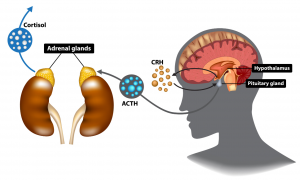
The adrenal glands are glands situated on top of the kidneys, as shown in the image below. They produce hormones and other chemicals that help regulate our responses to stress, as well as other essential functions including assisting blood pressure regulation, immune system and metabolism.
There is a communication pathway between the hypothalamus-pituitary in our brain, and the adrenal glands, known as the HPA-axis. The hypothalamus is the brain’s main regulator of our body and one of its most important functions is to link the nervous system to the endocrine system via the pituitary gland. When stress is perceived, it stimulates the pituitary gland (master hormone regulator) which in turn stimulates the adrenal glands, causing the release of adrenaline, our flight-fight hormone, followed by cortisol, our stress hormone.
To illustrate, imagine you are peacefully walking through the bush and a lion suddenly jumps out in front of you. Your instant reaction will be to get away (flight) and immediately a signal through the HPA axis instructs the adrenals to release adrenalin and cortisol assisting a fast get away from the situation. Once you are safe, your adrenal rhythm should normalise and recover after a while.
What is the function of cortisol in the body?
Some of the primary functions of cortisol under normal circumstances are:
- To provide instantaneous support during acute stressful situations by: a) Flooding the body with glucose as fuel for your muscles and brain, and b) Strategically constricting the arteries, to ensure more blood is available in the areas needed to deal with the fight-or-flight situation (legs, arms, heart, brain and lungs).
- Blood sugar regulation – it helps to maintain blood glucose concentrations by increasing gluconeogenesis (a breakdown process of protein and fats to glucose) and by blocking the uptake of glucose into tissues other than the central nervous system.
- Anti-inflammatory support – cortisol has an anti-inflammatory action by inhibiting the immune system which in turn inhibits production and action of inflammatory cytokines. Cytokines are molecules released by the immune system in response to inflammation, infection or trauma.
- Cortisol increases availability of all fuel substrates by mobilization of glucose, free fatty acids, and proteins from endogenous stores so that more energy can become available
Cortisol has a diurnal rhythm throughout the day, it should be high in the morning, spike after the first 30 minutes of waking, and decline during the day so that you have a lower level at night in order for your sleep hormone melatonin to be released. This rhythm gets affected when your stress is ongoing and your adrenal glands don’t get the chance to recover.
What happens when cortisol levels remain high for extended periods?
In our daily lives, sudden wildlife encounters are rare (phew!), however many of us experience constant physical and/or emotional stress. Physical stress can be caused by bodily conditions and symptoms, such as chronic pain, inflammation, infection, obesity or sugar imbalance. Emotional stress is caused by high-pressure jobs, working long hours, being a busy mom, experiencing personal family or relationship stress, and PTSD (post-traumatic stress disorder). All these experiences, whether emotional or physical, cause the brain to continually ask the adrenals to release cortisol, leading to constant high levels of cortisol in the body, and recovery time for the adrenal glands diminish.
In the short to medium term (Phase 1), chronically high cortisol leads to the following imbalances:
- Increased inflammation – cortisol has an anti-inflammatory effect during an acute stress situation however when cortisol is chronically high due to long term stress it can lead to inflammation. Prolonged stress alters the effectiveness of cortisol to regulate the inflammatory response because it decreases tissue sensitivity to the hormone. Specifically, immune cells become insensitive to cortisol’s regulatory effect. Latest research indicates that inflammation has been strongly implicated in fatigue and in behavioural withdrawal. (Dantzer et al., 2008; Miller and Raison, 2016))
- Blood sugar dysregulation due to the mobilisation of sugar from the tissue, which can lead to increase of sugar in your blood, leading to an increased release of insulin from the pancreas. Continuous high levels of insulin in the blood renders the cells in the blood less sensitive to the insulin, effecting its activity and leading to insulin resistance. This can lead to Type 2 diabetes.
- Poor sleep – difficulty falling asleep and waking up during the night. High cortisol levels impact our diurnal rhythm which can lead to a reduced release of our sleep hormone melatonin leading to difficulty to fall asleep and waking up during the night.
- Weight gain – When in excess, cortisol is an overall catabolic hormone, which decreases lean body mass and muscle mass and increase appetite and food intake. Insulin resistance also leads to weight gain and difficulty to lose weight.
- Overload on the thyroid gland – since the hypothalamus and pituitary glands also direct the thyroid function, an overstimulation of the HPA axis can therefore impact the thyroid function leading to hypothyroidism.
- Reduced immune system – this can develop from cortisol’s continual immune suppressive effects when abnormally high for long periods. This may be linked to increased tendency to develop auto-immune disease. When under stress, cells of the immune system are unable to respond to hormonal control, and consequently, produce levels of inflammation that promote susceptibility to disease.
In the medium to longer term (Phase 2), in other words if the situation described above is allowed to continue without any remedy or relief, and increased cortisol levels persist for months or years, a complicated dysregulation in the communication in the HPA axis develops, and counterintuitively, cortisol actually starts to decline below the levels which are required for healthy bodily functions, which leads to the following symptoms:
- Chronic exhaustion
- Feeling overwhelmed
- Poor emotional, mental, or physical resilience
- Weight gain, especially around the middle
- Difficulty to lose weight
- Frequent bouts of illness
- Low stress tolerance
- Anxiety, depression and irritability
- Poor mental function
- Sugar cravings
- Menstrual irregularities
What can be done to restore the balance?
The adrenal and HPA axis function can be improved and restored with the correct nutritional and adaptogenic herbal support, as well as lifestyle changes and/or stress management support.
The overactivity of the HPA axis and adrenal system creates an increased demand in the body for nutrients such as vitamin B5, Vitamin C and magnesium, therefore these levels need to be replenished. When your body is still in the high stress situation and the cortisol level is high (Phase 1), nutrients such as GABA, L-Theanine, magnesium and Phosphatidyl serine can help calm down the nervous system. On the other hand, when you have reached the stage where your cortisol has declined (Phase 2) and you are feeling completely exhausted and overwhelmed, adaptogenic herbs 4
and nutrients can help improve your response to stress and promote recovery. Evidence based studies show the efficacy of adaptogens on fatigue and their mechanism on stress protective activity (Alexander Panossian* and Georg Wikman, 2009).
Changes in lifestyle and stress management support is essential to support this recovery process so that you can reprogram your HPA axis to not immediately go into overdrive, and to return back to your normal rhythm when you have experienced acute stress.
The first step would be to test your cortisol levels to determine what your diurnal rhythm is doing during the day and if you have too high or too low cortisol levels. This is a service I provide to my patients and I will be providing more information in a next article/video about the test: Cortisol Awakening Response.
References:
https://www.britannica.com/science/cortisol
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5568897
https://www.researchgate.net/publication/228160384_Cortisol_and_physical_exercise
https://www.sciencedaily.com/releases/2012/04/120402162546.htm
https://www.researchgate.net/profile/Alexander_Panossian2/publication/26270136_Evidence-Based_Efficacy_of_Adaptogens_in_Fatigue_and_Molecular_Mechanisms_Related_to_their_Stress-Protective_Activity/links/00b49521093718d8e9000000/Evidence-Based-Efficacy-of-Adaptogens-in-Fatigue-and-Molecular-Mechanisms-Related-to-their-Stress-Protective-Activity.pdf?origin=publication_detail
Share this Post

